COVID-19 Update August 8, 2020
- icshealthsciencejournal

- Aug 8, 2020
- 3 min read
This article contains:
Monoclonal Antibody Trials May Beat Vaccines as Treatment for COVID-19
Monoclonal Antibody Trials May Beat Vaccines as Treatment for COVID-19
Written By: Paphapin Pairojtanachai
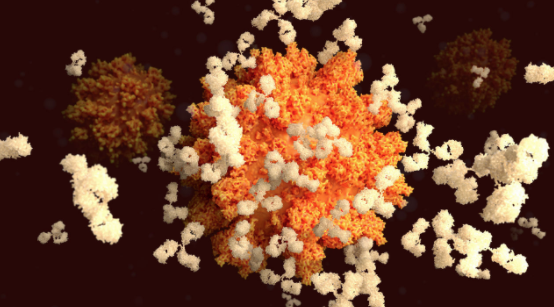
During the race to develop a vaccine for COVID-19, scientists are also trying to produce antibodies that could target the SARS-CoV-2. Antibodies are immune system proteins that work by binding and “neutralizing” the proteins on the surface of the virus, preventing them from initiating infection. Clinical trials are already underway, and synthetic monoclonal antibodies (mAbs) may be ready for usage as treatment in a few months, possibly even before vaccines become available.
On Tuesday, August 4, the National Institutes of Health (NIH) and Eli Lilly and Company announced the launching of two clinical trials for the inspection of mAbs and other experimental therapeutics. One of the trials will involve outpatients with mild symptoms, while the other will involve hospitalized patients. In patients diagnosed with mild or moderate COVID-19, the trial aims to determine if the antibodies can shorten the severity of the disease. In hospitalized patients, the study will determine the safety and efficacy of the antibodies. This news is the latest effort from the NIH’s Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) program, which was launched back in April “to speed development of the most promising treatments and vaccine candidates.”
The phase 2 clinical trial for mildly affected patients is called ACTIV-2. The LY-CoV555 antibody is the first therapeutic that will be tested. This mAb was found in the blood sample of a recovered COVID-19 patient by British Columbia–based AbCellera Biologics in collaboration with the Vaccine Research Center of the National Institute of Allergy and Infectious Diseases (NIAID). Following this discovery, Eli Lilly and Company joined the collaboration to manufacture the antibody.
For this ACTIV-2 trial, about 220 infected volunteers will be recruited: half of them will receive an intravenous infusion of LY-CoV555 and the other half will receive a placebo saline solution. All participants will be closely investigated over a period of 28 days to track their symptoms, check whether the coronavirus is still detectable, and observe how the treatment affects the course of their infection as well as how it functions in their bodies. If successful, the trial will transition into phase 3 with a total of 2,000 participants in order to study whether the experimental therapeutics can prevent hospitalization and/or death. NIH director Dr. Francis Collins expects that the researchers should know whether the therapy works or not by October or November.
As for hospitalized COVID-19 patients, the trial known as ACTIV-3 is already in phase 3 and is expanded to test multiple different types of mAb treatments. This randomized, controlled trial has an adaptive two-stage design that allows for flexibility, so that new therapeutics can enter the trial either at stage 1 or stage 2. The trial will be done in a similar way to ACTIV-2, but with approximately 300 patients. The participants will receive standard care for COVID-19 with antiviral drug remdesivir, and they will be assessed for needs of supplemental oxygen or mechanical ventilation. They will also be followed for a longer period of 90 days. Once again, if the trial is effective, more volunteers, including those who are severely affected by COVID-19, will be enrolled. The main goal is for the patients to be able to maintain their recovery for at least 14 days after hospital discharge.
During these clinical trials, data will be shared among both ACTIV-2 and ACTIV-3 examinations. As Anthony S. Fauci, the director of NIAID, notes, “Studying the impact of this investigational therapeutic on multiple patient populations at the same time is critical to determining whether it can help COVID-19 patients with differing levels of disease severity. These concurrent trials have the potential to yield significant and comprehensive clinical data.”
These monoclonal antibody tests are very important because they “have the potential to be an important bridge until the vaccine is available,” says Ajay Nirula, a vice president at Eli Lilly. Currently, there are good medications for COVID-19, but only for patients who are in the late stages of the disease. For instance, remdesivir is administered in hospitalized patients with lung disease, and dexamethasone is given to patients who require oxygen and ventilation. The purpose of the antibodies, however, is for use in both outpatients and inpatients who aren’t under severe conditions. In addition, the mAbs can also be used as protection for healthcare workers under high risk of acquiring the disease.
The ACTIV-2 and ACTIV-3 tests aren’t the only ongoing clinical trials. There are hundreds more that are experimenting on a variety of different antibodies, and this provides a thousand opportunities for a potential weapon against COVID-19.






Comments