COVID-19 Update April 15, 2020
- icshealthsciencejournal

- Apr 15, 2020
- 4 min read
Updated: May 6, 2020
This article contains:
Using Convalescent Plasma to Treat the COVID-19
Coronavirus Reactivation & Other Problems in Recovered/Asymptomatic Patients
Using Convalescent Plasma to Treat the COVID-19
Written By: Kandharika Bamrungketudom

During the time of waiting for vaccines and medications that can cure the COVID-19 to develop, doctors have turned to using the plasma of the recovered patients as a form of treatment for the COVID-19 patients.
This method had been utilized since the 1890s to treat the flu pandemic, but also other diseases such as measles, chickenpox, and Ebola.
The reason as to why this method works is that the plasma of a patient that has recently recovered from the COVID-19 contains antibodies. Patients who have recently been infected with the coronavirus, however, will not have antibodies for the coronavirus yet. Transfusing the plasma from the recovered patients — and therefore their antibodies — into the person newly infected with the coronavirus may help speed up the recovery.
Data collected from 10 COVID-19 patients in China that had received plasma infusion shows hopeful signs that plasma can indeed treat the COVID-19. In this study, 10 severe adult patients (ages from 34-78) were given a dose of convalescent plasma (plasma from a recovered patient, also known as CP). This study has shown a positive result, with the clinical symptoms of the COVID-19 improving within 3 days and the virus within the bloodstream of the patients disappearing at around 7 days after the plasma was transfused. However, more research and data has to be gathered before it could be said with certainty that the convalescent plasma can treat the infected patients.
One reason for the uncertainty in the data is that there are many variables in the plasma each patient receives, since the sources where the plasma is collected differ. Because of the variability in the composition of the plasma each patient receives, it can be difficult for researchers to tell whether the plasma is generally effective or whether it depends on the other composition of immune substances in the plasma as well.
Another reason as to why this method of treatment is not so readily administered is that serious side effects that can cause lung injuries and allergic reactions can occur.
However, if the convalescent plasma can indeed help people recover from the COVID-19, it may also prepare the doctors towards a treatment for the second wave of the disease, should it occur, and it is also a way of treating the COVID-19 patients, until more drugs could be developed.
Coronavirus Reactivation & Other Problems in Recovered/Asymptomatic Patients
Written By: Paphapin Pairojtanachai
A week ago, there were case reports in South Korea in which 51 people who had recovered from COVID-19 tested positive for the novel coronavirus for a second time. On Monday, April 13, 2020, South Korea reported an addition of over 100 of such cases. This raised concerns about releasing patients out of hospitals and stamping out infections. While health officials are still researching for the cause of these relapses, Dr. Jeong Eun-kyeong, director of the Korea Centres for Disease Control and Prevention (KCDC), suggested that the patients may not have been reinfected, but instead the coronavirus may have been “reactivated”.
The reactivation of the virus is due to the possibility that there are still residuals of the virus lingering in the recovered patients, alike cases for the Herpes virus and the HIV. These patients were, however, thought to be recovered because the amounts of virus per milliliter of their blood were very low. Since the coronavirus tests are not sensitive enough, they resulted as negative even though the virus still lay dormant in the patients’ bodies.
Researchers are still studying whether the coronavirus “remains” stay inactive in the body or whether they become activated under certain conditions, as well as what damage the virus can do to the body, both in dormant and active states. Similar cases have been reported elsewhere, including China. Furthermore, there are cases of those who got reinfected despite having recovered and having the antibodies specific for the virus. This led to theories that developed immunity and antibodies for the coronavirus could be short term.
Currently, the WHO advises that COVID-19 patients should be tested negative for two consecutive times, with at least 24 hours in between the tests, before they can be discharged from the hospital. The members said, “We are closely liaising with our clinical experts and working hard to get more information on those individual cases. It is important to make sure that when samples are collected for testing on suspected patients, procedures are followed properly.”
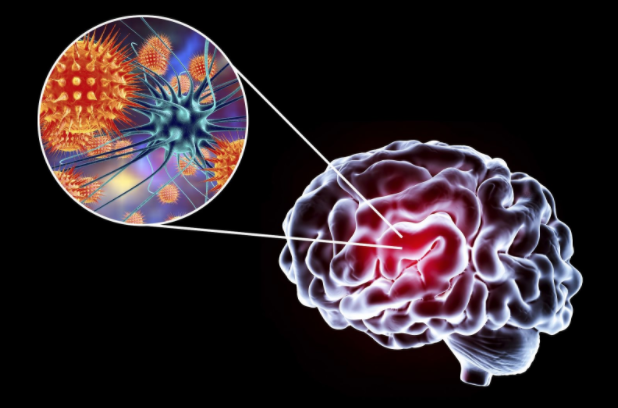
Apart from the reactivation of the novel coronavirus, medical researchers from the University of California San Diego School of Medicine have warned that healthcare professionals should be aware of neuropsychiatric problems that may emerge in patients who have recovered or who are asymptomatic (those who do not show symptoms). Dr Emily A. Troyer (a professor from the Department of Psychiatry of UC San Diego School of Medicine) said, "Past pandemics have demonstrated that diverse types of neuropsychiatric symptoms, such as encephalopathy, mood changes, psychosis, neuromuscular dysfunction or demyelinating processes, may accompany acute viral infection, or may follow infection by weeks, months, or longer in recovered patients." There are also reports of symptoms associated with the central nervous system (CNS) in COVID-19 infected patients, including temporary loss of smell and taste senses.
Additionally, COVID-19 is a source of stress due to fears of illness, death, and uncertainty for the future, as well as economical issues and social problems within communities. This could lead to insomnia, anxiety, depression, mania, delirium, or even suicidal acts. In spite of this potential traumatization, not much attention has been focused on how the novel coronavirus affects the human nervous system. The researchers from the Departments of Psychiatry and Family Medicine and Public Health at UC San Diego School of Medicine mentioned that although the consequences of these problems are still unknown, they will likely be significant and long-lasting. Therefore, they recommend that medical workers should keep an eye on neuropsychiatric conditions in people exposed to the coronavirus.








Comments